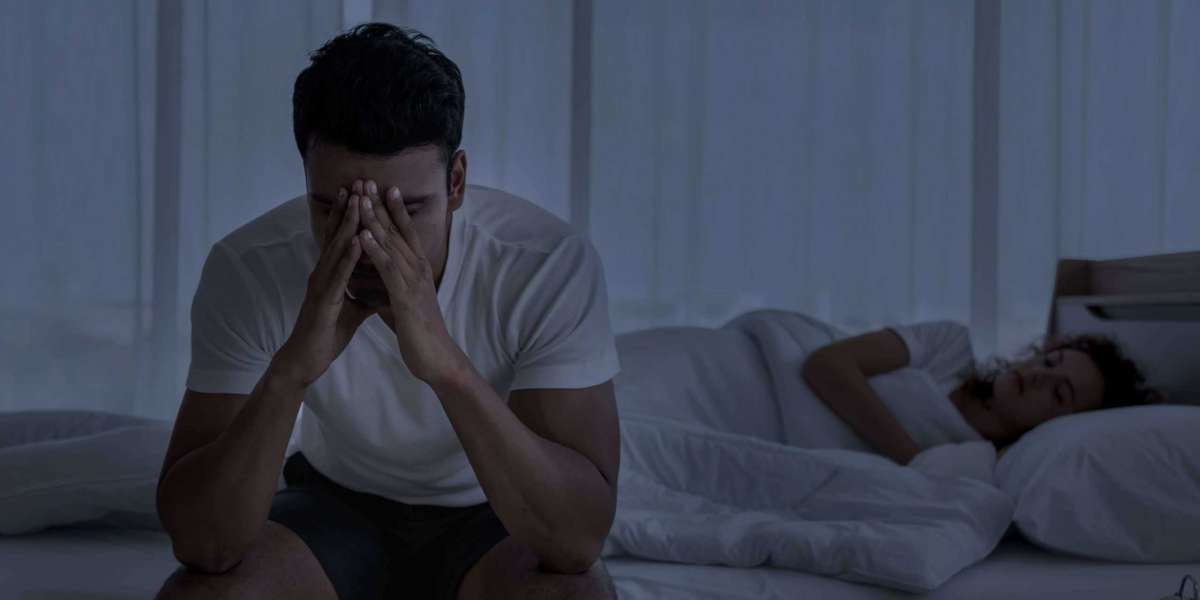
Millions of people worldwide suffer with insomnia, a common sleep problem marked by difficulty falling asleep, staying asleep, or both.
Millions of people worldwide suffer with insomnia, a common sleep problem marked by difficulty falling asleep, staying asleep, or both. Though research indicates a considerable gender discrepancy in its occurrence and appearance, it can affect anyone, regardless of gender. So the question is: Do women experience insomnia at higher rates than do men? This article explores the complex relationship between gender and insomnia and the causes that may be causing this gap.
Knowing About Sleeplessness:
Prior to exploring gender variations, it is important to understand the basics of insomnia. The term "insomnia" refers to a range of symptoms, including trouble falling asleep, difficulties staying asleep, and early morning awakenings. Its effects do not stop at night; they frequently cause weariness, difficulty concentrating throughout the day, and emotional instability, all of which severely lower one's quality of life. Differences in Prevalence:
Research continuously shows that women experience insomnia at a higher rate than men. According to a meta-analysis that was published in Sleep Medicine Reviews, women are 40% more likely than males to experience insomnia. In addition, a study conducted by the National Sleep Foundation indicates that roughly 1 in 4 women and 1 in 5 men report having symptoms of insomnia.
The gender gap in insomnia may be caused by a number of biological causes. Women's sleep patterns are greatly impacted by hormonal shifts, especially those related to the menstrual cycle, pregnancy, and menopause. An increased susceptibility to insomnia can result from the disruption of the sleep-wake cycle caused by the change of estrogen and progesterone levels during these phases.
Furthermore, studies suggest that gender-specific variations in brain structure and function might be involved. Research employing neuroimaging methods has revealed differences in the brain circuits responsible for regulating sleep, which may make women more prone to sleep disruptions.
Gender variations in insomnia are largely shaped by psychosocial factors. Women are frequently under more pressure to balance numerous tasks, such as caregiver, housewife, and professional, due to societal standards and expectations, which raises stress and anxiety levels. Persistent stress has the potential to worsen sleep difficulties, therefore creating a vicious cycle of insomnia.
among addition, mood disorders like anxiety and sadness, which are directly linked to sleeplessness, are more common among women. Women's symptoms of insomnia are further aggravated by the reciprocal relationship between mental health and sleep, which results in a complicated interaction between biological and psychosocial factors.
Environmental and Lifestyle Factors:
Both the amount and quality of sleep are strongly influenced by environmental factors and lifestyle decisions. Stress at work, domestic tasks, and caregiving responsibilities may make women more likely to develop poor sleeping patterns. Furthermore, women may prioritize exercise or grooming routines over sleep due to cultural expectations around beauty and body image, which could further compromise their sleep hygiene.
Furthermore, during major life transitions like pregnancy, childbirth, and menopause, women are more likely to have sleep disruptions. Hormonal fluctuations in addition to these physiological changes might cause sleep patterns to be disturbed and symptoms of insomnia to worsen.
Although women are more likely than males to experience insomnia, there is a discernible gender difference in the availability and acceptance of suitable therapy. According to research, there are a number of reasons why women are less likely than males to seek medical attention for sleep-related problems, including social barriers, lack of understanding, and stigma.
Furthermore, rather than identifying and treating underlying sleep disorders, medical professionals may undervalue or misinterpret women's sleep complaints, attributing them to psychological or hormonal swings. Women who experience insomnia may not receive the proper care or attention because of this under recognition. Diversity and Intersectionality: It's critical to understand that, in addition to gender, there are differences in insomnia experiences according on race, ethnicity, socioeconomic background, and other intersecting identities. Studies with a broad sample size can provide insight into the ways in which a number of variables interact to affect the disparities in sleep health. Interventions can be designed to target the particular obstacles to sleep health in each community by taking into account the particular requirements and difficulties that each group faces.
Sleep Issues Other Than Insomnia:
Even though insomnia is the most common sleep problem, both the quantity and quality of sleep are affected by other sleep disorders as well, including sleep apnea, restless legs syndrome, and circadian rhythm disturbances. More research is necessary to determine whether gender variations exist in the prevalence and expression of these illnesses. Gaining knowledge about the ways in which gender interacts with various sleep disorders might help design more focused interventions and enhance outcomes for both genders.
Studies that follow people over the course of their lives might offer important insights about how insomnia develops and how it affects health outcomes over time. Through the study of the changes in sleep patterns from childhood to adolescent to maturity and beyond, researchers may pinpoint vulnerable times and develop early intervention plans. Additionally, longitudinal data can clarify the ways in which gender-specific factors influence the onset and course of insomnia over the course of a person's lifetime. Integrative techniques are crucial for managing insomnia since they acknowledge the intricate interactions between biological, psychological, and environmental components. Integrative methods have demonstrated potential in improving sleep outcomes. These interventions combine pharmaceutical treatments with mindfulness-based therapies, cognitive-behavioral therapy for insomnia (CBT-I), and lifestyle adjustments. Interventions can be made more successful and encourage long-term adherence by being specifically designed to meet the needs and preferences of women.
There is a gender gap in insomnia, which is a complex phenomenon impacted by environmental, psychological, and biological factors. Insomnia affects women more than males, but the underlying causes are intricate and multifaceted. In order to address this difference, a comprehensive strategy that guarantees equal access to diagnosis and treatment while acknowledging the particular difficulties women encounter in sustaining healthy sleep patterns is needed.
We may work to close the gender gap in insomnia and enhance everyone's sleep health by increasing awareness, advocating gender-sensitive healthcare practices, and addressing cultural norms that contribute to sleep disorders. In the end, gender equality in sleep health requires cultivating a culture that values sleep as an integral part of general wellbeing.
 Balenciaga フーディーブラック コットン シ
By Tyra Moss
Balenciaga フーディーブラック コットン シ
By Tyra Moss The Enigmatic World of Hong Kong Escorts: Unveiling the Fascination
By Adah Fadel
The Enigmatic World of Hong Kong Escorts: Unveiling the Fascination
By Adah FadelDiscover the Perfect Scam Verification Platform with Casino79 for Your Toto Site Experience
 Top Models & Companionship in Dubai
By Ann Bugatti
Top Models & Companionship in Dubai
By Ann Bugatti Prepare For The Pleasure With Bahrain Escort Services
By Ann Bugatti
Prepare For The Pleasure With Bahrain Escort Services
By Ann Bugatti