With the fight against cervical cancer continuing, a considerable change has been realized, stating a new leaf that should be witnessed in the efforts that should be aligned to the methods of prevention and screening protocols. Central to this change is the validation of the Human Papillomavirus (HPV) as the basic etiological agent and not just a co-factor for the etiology of cervical cancer. This central behavior has sparked a lot of innovations in the delivery and coverage of cervical cancer screening; today, updated guidance stresses the necessity of having the HPV test in place.
These revisions are based on accumulated evidence from years of research activities and emerging uniformity among the clinical and other healthcare personnel on the desirable approaches to screening and preventing cervical cancer. As we address the highlights on the effects of these updates on such guidelines, below is a clear understanding from the best cancer hospital in India of what links HPV and cervical cancer and what the recommendations entail, and globally for women as well. This blog sets out to articulate these advancements, revealing how they characterize a dynamic push ahead to ensure ladies’ health.
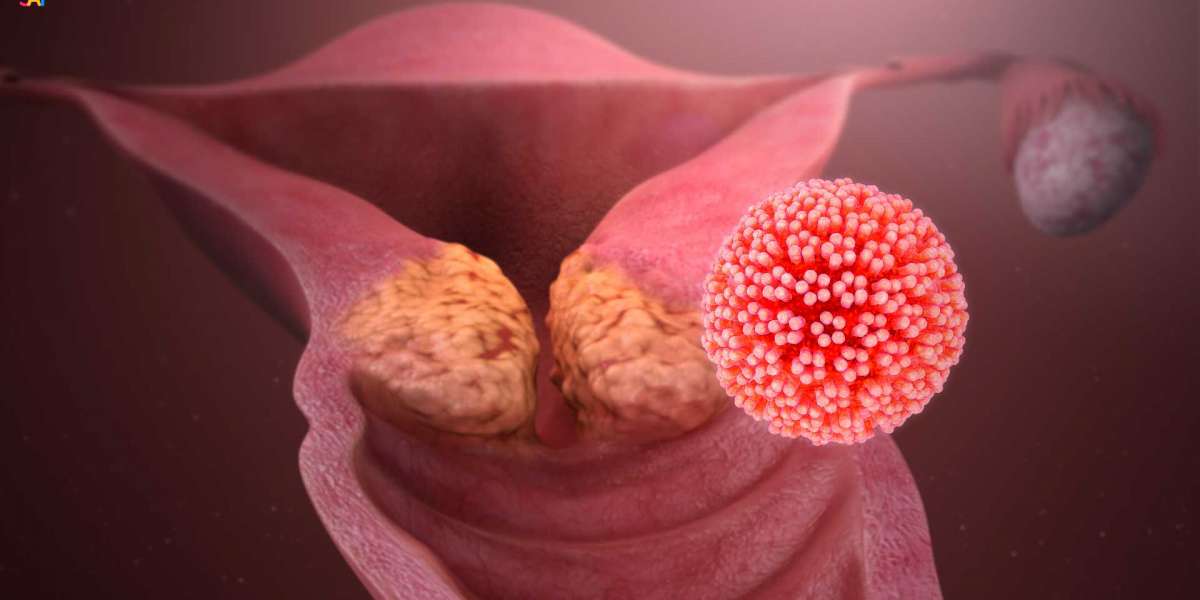
What is HPV?
The human papillomavirus comprises a group of viruses that have more than 200 related diseases, but moreover, there are more than 40 types of related diseases that are easily transmitted by sexual contact. Although the majority of them cause no consequences for human health and clear up on their own, sustained infection with the high-risk HPV types results in the development of cervical cancer.
HPV and Cervical Cancer
In excess of 40 of HPV's 200 types can be transmitted sexually. It is the most prevalent sexually transmitted disease worldwide for people of both genders. Notwithstanding the presented frequency, a considerable number of people are not aware of it or its significant health consequences. This part discusses what HPV is, HPV types, modes of transmission, and their links with various types, as well as cervical cancer.
Transmission
HPV is basically transmitted through sexual contact, counting vaginal, butt-centric, and verbal sex. It can be passed indeed when a contaminated individual has no signs or indications. In uncommon cases, it can also be transmitted from a pregnant lady to her child during childbirth.
HPV Infection and Its Course
Most HPV contaminations are asymptomatic and resolve suddenly without causing any wellbeing issues. Be that as it may, when the infection does not clear, it can lead to the advancement of genital warts or cancerous injuries, depending on the HPV sort included. The body's resistant system decides whether an HPV disease will clear or lead to more serious conditions.
HPV and Cancer
The mechanism by which high-risk HPV sorts lead to cancer includes the integration of HPV DNA into the heart cell's DNA. This integration disturbs cell growth's typical control, driving cancerous cell advancement. Persistent disease with high-risk HPV sorts could be a figure for the improvement of cervical and other anogenital cancers, as well as a subset of head and neck cancers.
Prevention
Prevention of HPV infection is conceivable through inoculation. HPV immunization is viable against the foremost common high-risk and a few low-risk sorts of HPV. It is suggested that preteens (boys and girls) mature from 11 to 12 for a long time but can be managed as early as 9 and up to age 45 in a few cases. The antibody is most compelling when, sometime recently, a person gets to be sexually active.
Screening and Early Detection
For cervical cancer, customary screening through Pap smears and HPV testing is significant. Pap smears can distinguish pre-cancerous and cancerous cells within the cervix, whereas HPV testing distinguishes the nearness of high-risk HPV sorts. Together, these screening methods are effective instruments for the early location and avoidance of cervical cancer.
Recent Guideline Changes
The most recent rules emphasize the significance of HPV testing in cervical cancer screening. Key changes incorporate:
- HPV Testing as a Primary Screening Tool: Numerous rules presently suggest HPV testing as the essential strategy for cervical cancer screening instead of depending exclusively on Pap smears. This shift reflects HPV's part in the majority of cervical cancer cases.
- Starting Age and Screening Intervals: The age to start screening has been overhauled in numerous rules, with a proposal to begin HPV testing at age 25 or 30, depending on the particular rules. Also, the interim between screenings has been expanded to each five a long time in case HPV testing is utilized, recognizing the virus's moderate movement to cancer.
- Co-testing: Some guidelines suggest a co-testing approach, combining HPV testing with a Pap smear, for a transitional period. This dual approach can provide a more comprehensive screening outcome.
Implications of the Guideline Changes
- Increased Detection: Early detection, with the help of the Best cancer hospital in India, of high-risk HPV sorts can distinguish women at hazard for cervical cancer. Sometime recently, cancerous or pre-cancerous cells develop.
- Prevention of Over-treatment: By focusing on the discovery of high-risk HPV, pointless medications for injuries likely to resolve on their own can be maintained at a strategic distance, lessening the hazard of unfavorable impacts from such treatments.
- Vaccination Awareness: The accentuation on HPV's part in cervical cancer highlights the significance of HPV immunization for anticipation. Immunizations can secure against the sorts of HPV most commonly connected to cervical cancer.
Challenges and Considerations
While the shift towards HPV testing is a positive step, it also brings challenges:
- Access and Awareness: Ensuring that all ladies have access to HPV testing and get the changes in rules is crucial.
- Vaccine Hesitancy: Tending to immunization aversion and deception about HPV immunization is basic for avoidance efforts.
- Global Disparities: Executing these rules all-inclusive, particularly in low-resource settings where cervical cancer rates are most noteworthy, and HPV immunization rates are low, remains a challenge.
Conclusion
The new changes in the guidelines for cervical cancer screening are about more than just how we do things; they demonstrate a change in how we think about cervical cancer and its prevention. In shifting their strategy to put HPV testing at the center of screening programs aimed at early detection and administration to initiate an epoch of informed, effective screening strategies, these guidelines change the narrative. Such a change in screening practices supports the idea of the necessity of public awareness and the popularity of vaccination against HPV as a way to address this problem and decrease the number of cervical cancer cases.
Nonetheless, the voyage continues after the publication of the new guidelines. The real challenge lies in implementation: to make certain that all women receive HPV screening, comprehend the changes, and empower themselves to lead a healthy lifestyle. It also includes scaling it up to overcome issues with barriers, addressing vaccine hesitancy, and closing the global gap in access to screening and vaccination.